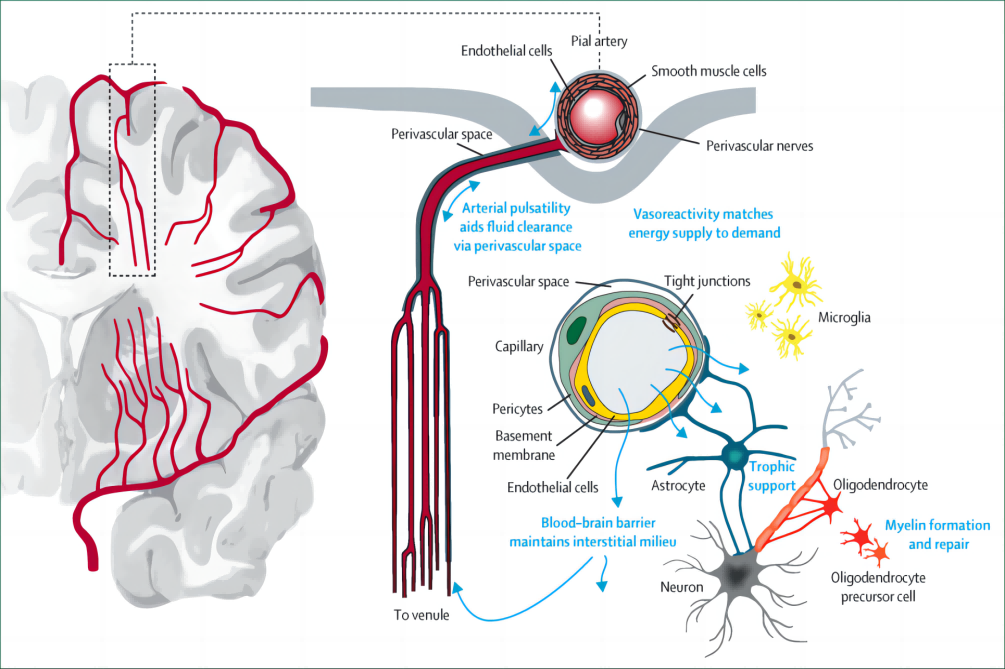
Cerebral small vessel disease (CSVD) refers to a group of diseases whose pathological changes mainly involve small blood vessels deep in the brain. It can be roughly divided into simple and complex categories. The vascular lesions of simple CSVD are mainly lipid hyalinization of the vessel wall; complex CSVD has a greater degree of damage to the vessel wall, and necrosis of the interstitium, collagen fibers and small vessel walls - fibrinoid necrosis.
clinical manifestations
The lesions of CSVD are small, and patients are often not aware of it until obvious symptoms appear. Symptoms can include stroke, bleeding, dementia, cognitive impairment, depression, balance disorders and urinary incontinence. Data show that there are 30,000 cases of stroke caused by CSVD in the UK every year, while there are 600,000 to 700,000 cases in China.
Clinical manifestations of CSVD also include recent small subcortical infarcts or asymptomatic cerebrovascular disease. CSVD also has some "silent" features, such as microinfarcts, focal or widespread atrophy, and hemorrhage, which are more common in the elderly.
Imaging manifestations
The imaging appearance of small subcortical infarctions in the acute phase is variable and may indicate different lesions. Larger infarcts are more likely to indicate cerebral arterial disease and arterial stenosis; smaller ones may indicate internal lesions of small blood vessels. In addition, the long-term manifestations of CSVD are also very diverse. 10% of the lesions disappear after 1 year, 30% to 70% appear similar to white matter hyperintensity (WMH), and 20% to 94% transform into cysts.
Generally speaking, CSVD is believed to develop and worsen gradually. The 3-year follow-up results of imaging studies show that the volume of WMH increases by an average of 1.5% per year. There are population differences in this process. If the risk factors are well controlled, the development rate of WMH can be much lower than 1.5%. In fact, WMH can also disappear gradually, that is, CSVD is not necessarily a permanent lesion.
risk factors
85% of CSVD originates from lesions in the small blood vessels themselves, and its risk factors include typical vascular disease risk factors such as hypertension, diabetes, smoking, and cholesterol levels. Research shows that the importance of some known risk factors, such as smoking, may be underestimated. Some studies have also shown that salt intake, arteriosclerosis, lack of exercise, and blood-brain barrier damage are related to CSVD.
Damage mechanism of CSVD
The damage mechanism of CSVD may be an increase in the permeability of the cell wall in the inner wall of small blood vessels, and proteins and other substances in the blood enter the blood vessel wall, causing thickening and disintegration of the vessel wall. Thickening of blood vessel walls or entry of plasma and other substances into the brain parenchyma can cause damage to adjacent brain tissue, and thrombosis occurs in the late stages as a secondary pathological change.
treat
Based on the above theory of CSVD injury mechanism, it means that its potential therapeutic target is abnormal endothelial function, but traditional treatments are not significantly effective.
The SPS3 trial showed that compared with aspirin monotherapy, aspirin combined with clopidogrel not only increased deaths, but also had no significant benefit in preventing stroke recurrence and cognitive function decline; intensive blood pressure lowering was less effective than guideline-based blood pressure lowering. There was no significant benefit in preventing stroke recurrence and cognitive decline. Other studies have shown that the impact of blood pressure lowering on WMH has mixed results. Although statins can slow down the decline of cognitive function, they are ineffective in preventing WMH. Vitamin B12-folic acid may be beneficial for severe WMH.
prevention
First, treat blood pressure, lipids, and antiplatelet drugs (but not long-term dual anti-drugs) according to the guidelines; second, intervene in the patient's lifestyle according to the consensus; finally, conduct new research, explore new and existing drugs, and produce More experimental animal data provide the basis for human studies.